Understanding Anti-Phospholipid Antibody Screening and the Importance of ELISA in Diagnosis
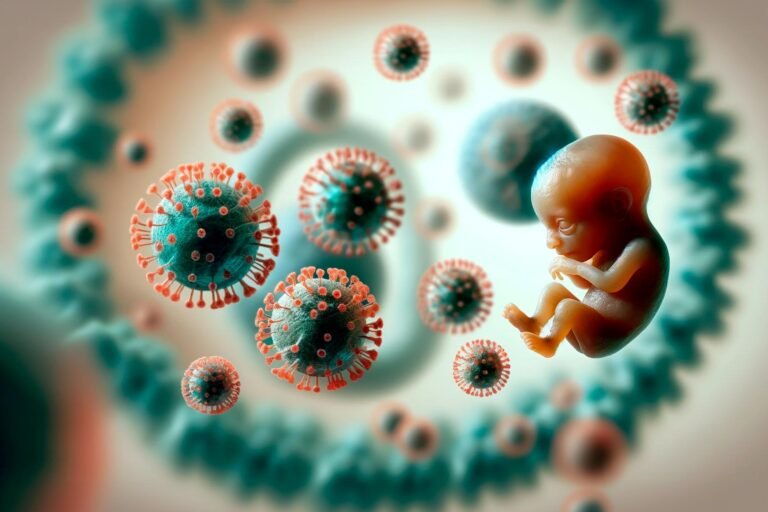
Introduction: Anti-phospholipid syndrome (APS) is an autoimmune disorder in which the immune system mistakenly produces antibodies against phospholipids, which are vital components of cell membranes. This condition increases the risk of blood clots, pregnancy complications, and other severe health issues. Early detection and diagnosis through anti-phospholipid screening, often using ELISA (Enzyme-Linked Immunosorbent Assay), are critical in managing APS effectively.
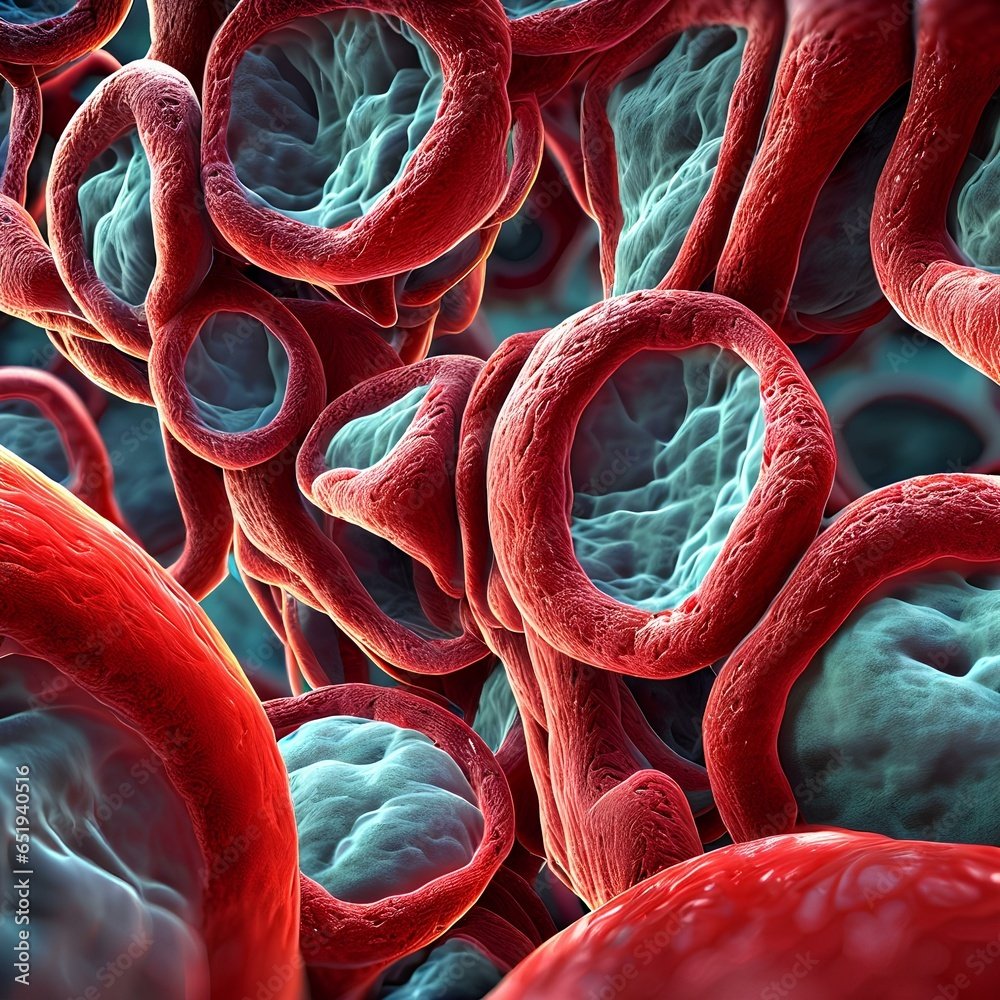
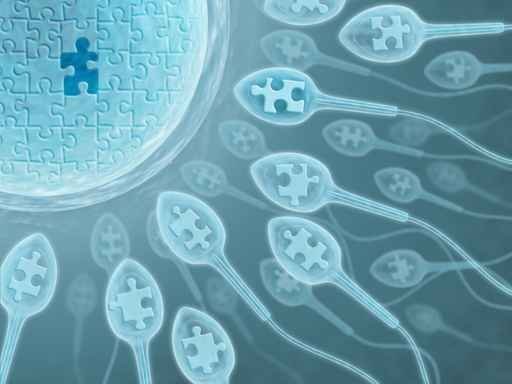
Clinical Significance of Anti-Phospholipid Screening: Anti-phospholipid antibodies (aPL) can target proteins like beta-2-glycoprotein I and prothrombin, essential in the coagulation system. The presence of these antibodies leads to a heightened risk of thrombotic events (e.g., deep vein thrombosis, pulmonary embolism) and pregnancy-related complications, such as recurrent miscarriages and preeclampsia. By detecting these antibodies early, healthcare providers can tailor treatment plans to mitigate these risks, especially for patients with known risk factors like systemic lupus erythematosus (SLE) or unexplained clotting events.
Types of Anti-Phospholipid Antibodies: Screening typically focuses on identifying three primary antibodies:
- Lupus Anticoagulant (LA) – Commonly associated with prolonged clotting times, indicating clotting risk.
- Anti-Cardiolipin (aCL) – IgG and IgM antibodies against cardiolipin, a significant phospholipid linked with thrombosis and pregnancy complications.
- Anti-Beta-2 Glycoprotein I – Antibodies specifically target beta-2-glycoprotein I, which strongly correlates with APS-related risks.
Importance of ELISA in Anti-Phospholipid Antibody Diagnosis: ELISA is a robust and widely accepted method for detecting and quantifying aPL. The assay’s principle involves immobilizing phospholipid antigens on a solid surface and detecting specific antibodies in a patient’s blood sample. ELISA offers several advantages:
- High Sensitivity and Specificity: ELISA’s sensitivity allows it to detect a broad range of antibody concentrations, making it ideal for identifying low levels of aPL that might otherwise go undetected.
- Quantitative Results: ELISA provides precise, quantitative measurements of antibody levels, helping clinicians assess the risk of APS. This quantification is crucial since higher antibody levels are often associated with a greater likelihood of thrombotic events.
- Consistency and Reproducibility: The standardized ELISA protocol provides reliable and reproducible results, reducing variability between different laboratories and ensuring that healthcare providers can trust the results for clinical decisions.
ELISA and Anti-Phospholipid Antibody Testing Protocol: The ELISA test protocol includes a few standardized steps to ensure accuracy. Blood samples are collected, and serum is separated to test for IgG and IgM classes of aPL. This dual-class testing is crucial as IgG is often more clinically significant, while IgM can indicate an active autoimmune response.
Healthcare providers should consider ELISA testing for:
- Individuals with unexplained thrombotic events, especially at a young age.
- Women experiencing recurrent miscarriages or preeclampsia.
- Patients with autoimmune conditions, particularly SLE, as they have an increased risk of APS.
Interpreting ELISA Results for APS Management: Positive results from anti-phospholipid screening via ELISA indicate the presence of aPL. For an official APS diagnosis, however, patients typically must test positive on two separate occasions, at least 12 weeks apart. This minimizes the risk of transient antibodies (often resulting from infections) being misinterpreted as APS-related.
Upon diagnosis, treatment options may include anticoagulants like warfarin or heparin to reduce clotting risk, especially for patients with a history of thrombosis. Low-dose aspirin may also be recommended for pregnant women with APS to prevent pregnancy complications.
Conclusion: Anti-phospholipid antibody screening through ELISA plays a vital role in diagnosing APS. The sensitivity, specificity, and quantitative nature of ELISA make it a valuable tool for identifying APS and enabling timely interventions that reduce the risk of serious complications. Through early detection and appropriate management, patients with APS can lead healthier, safer lives with reduced clotting risks and improved pregnancy outcomes.