Beta 2 Glycoprotein I: Clinical Significance and Its Role in Autoimmune Diseases
Beta 2 Glycoprotein I (β2GPI) is a multifunctional plasma protein that significantly regulates blood coagulation and lipid metabolism. It is particularly notable in the context of autoimmune diseases, especially antiphospholipid syndrome (APS). This blog explores the clinical significance of β2GPI, its involvement in autoimmune disorders, and the implications for diagnosis and treatment.
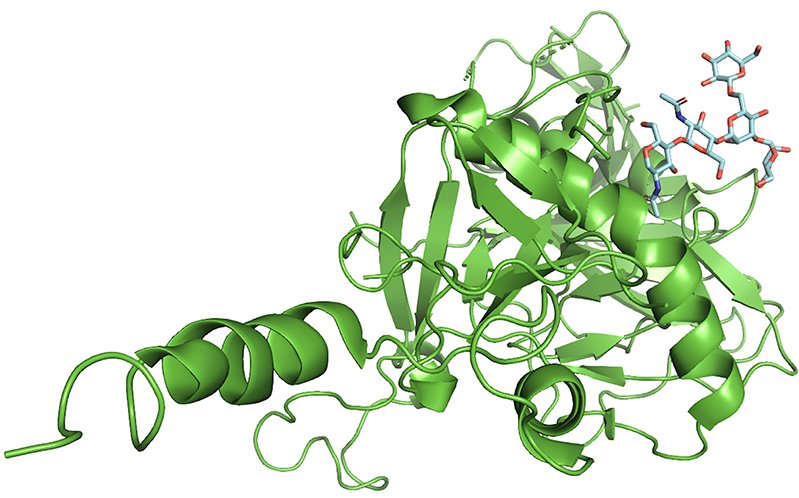
Understanding Beta 2 Glycoprotein I
Beta 2 Glycoprotein I is a 50 kDa protein predominantly synthesized in the liver and found circulating in the blood. It consists of five domains and exhibits several biological activities, including binding to anionic phospholipids and inhibiting pro-coagulant enzymes. This protein acts as a cofactor for the binding of antiphospholipid antibodies, which are implicated in certain autoimmune conditions.
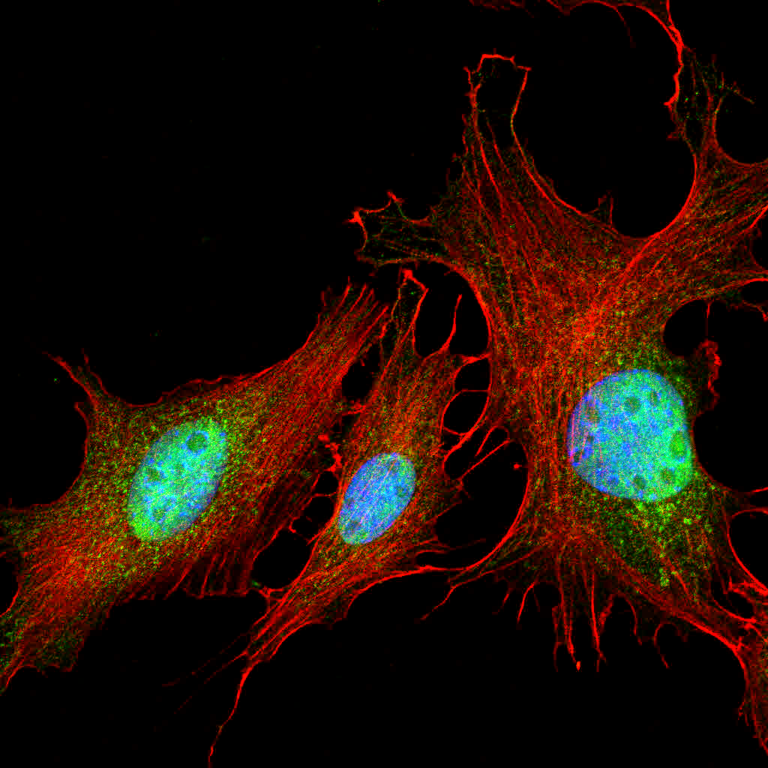
The Role of β2GPI in Autoimmune Diseases
The presence of autoantibodies against β2GPI is a key feature in various autoimmune diseases, most notably in antiphospholipid syndrome (APS). These autoantibodies can lead to severe clinical manifestations, including:
- Thrombosis: Autoantibodies against β2GPI promote the formation of blood clots in veins and arteries, increasing the risk of deep vein thrombosis, pulmonary embolism, and stroke.
- Pregnancy Complications: Women with APS often experience recurrent miscarriages, preterm delivery, and other pregnancy-related issues due to placental thrombosis and impaired placental function.
- Thrombocytopenia: The presence of anti-β2GPI antibodies can lead to a decrease in platelet count, contributing to bleeding disorders and complicating thrombosis.
Clinical Significance of β2GPI
- Diagnostic Marker: The detection of anti-β2GPI antibodies is crucial for diagnosing APS. These antibodies are considered more specific markers for APS compared to other antiphospholipid antibodies.
- Risk Stratification: Measuring levels of anti-β2GPI antibodies helps in stratifying patients based on their risk of developing thrombotic events and pregnancy complications. This enables tailored preventive strategies and treatments.
- Therapeutic Monitoring: Monitoring anti-β2GPI antibody levels can provide insights into the effectiveness of therapeutic interventions in patients with APS, guiding adjustments in treatment plans.
- Research and Development: Understanding the interactions and pathways involving β2GPI and its autoantibodies facilitates the development of new therapeutic approaches and enhances our knowledge of autoimmune disease mechanisms.
Diagnostic Techniques for β2GPI Antibodies
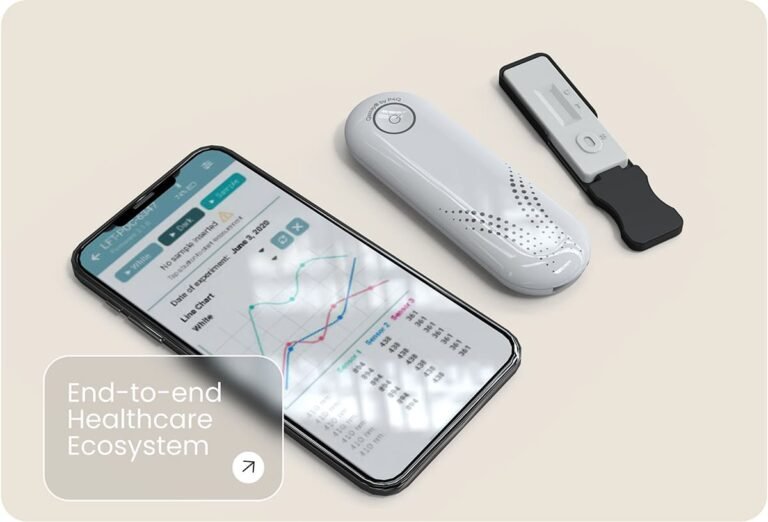
The primary method for detecting anti-β2GPI antibodies is the Enzyme-Linked Immunosorbent Assay (ELISA). This technique offers high sensitivity and specificity, making it the gold standard for diagnosing APS. The process involves:
- Sample Collection: Blood samples are collected from patients and processed to obtain serum or plasma.
- Antigen Coating: Microplate wells are coated with purified β2GPI antigen.
- Sample Addition: Patient samples are added to the wells. If anti-β2GPI antibodies are present, they bind to the antigen.
- Detection: A secondary enzyme-linked antibody specific to human antibodies is added, which binds to the patient’s anti-β2GPI antibodies.
- Substrate Reaction: A substrate is added, producing a color change proportional to the antibody concentration.
- Quantification: The intensity of the color is measured, providing a quantitative result of antibody levels.
Treatment and Management of APS
The management of APS involves anticoagulant therapy to prevent thrombotic events and address pregnancy complications. Common treatments include:
- Anticoagulants: Warfarin, heparin, and direct oral anticoagulants (DOACs) are commonly used to reduce clotting risks.
- Antiplatelet Agents: Aspirin is often prescribed to prevent clot formation.
- Immunosuppressive Therapy: In severe cases, immunosuppressive drugs may be used to reduce the production of autoantibodies.
Conclusion
Beta 2 Glycoprotein I is a pivotal protein with significant implications in autoimmune diseases, particularly antiphospholipid syndrome. Its role in the formation of autoantibodies and the resultant clinical manifestations underscore its importance in the diagnosis, risk assessment, and management of APS. Advanced diagnostic tools like the anti-β2GPI ELISA kit enhance our ability to detect and monitor this condition, ultimately improving patient outcomes. As research continues, a deeper understanding of β2GPI will likely lead to novel therapeutic strategies and better management of autoimmune diseases.