Clinical Significance and Diagnostic Importance of AMH (Anti-Müllerian Hormone)
Introduction
Anti-Müllerian Hormone (AMH) has emerged as a key biomarker in reproductive endocrinology and fertility medicine. Produced by the granulosa cells of ovarian follicles in females and Sertoli cells in males, AMH provides valuable insight into ovarian reserve, reproductive potential, and certain pathological conditions. Its stability throughout the menstrual cycle makes it a reliable indicator for evaluating ovarian function and reproductive health.
What Is AMH?
AMH is a glycoprotein hormone belonging to the transforming growth factor-beta (TGF-β) family. In women, AMH is secreted by small growing follicles (pre-antral and small antral follicles) in the ovaries. Its level directly reflects the quantity of remaining viable eggs (ovarian reserve).
In men, AMH is produced by Sertoli cells of the testes and plays a crucial role in male sexual differentiation during fetal development.
Clinical Significance of AMH in Women
1. Assessment of Ovarian Reserve
- AMH is one of the most reliable biomarkers for assessing ovarian reserve.
- Unlike FSH or LH, AMH levels remain relatively stable throughout the menstrual cycle.
- Low AMH levels indicate diminished ovarian reserve, which can impact fertility potential.
- High AMH levels may suggest polycystic ovarian morphology or hormonal imbalance.
2. Fertility Evaluation and IVF Prognosis
- AMH helps clinicians predict response to ovarian stimulation in assisted reproductive techniques (ART) like IVF and ICSI.
- Women with high AMH typically respond well to stimulation, while those with low AMH may require tailored treatment protocols.
- AMH helps avoid ovarian hyperstimulation syndrome (OHSS) by optimizing medication dosage.
3. Diagnosis of Polycystic Ovary Syndrome (PCOS)
- Elevated AMH levels are commonly observed in women with PCOS due to an increased number of small antral follicles.
- AMH can serve as a supportive diagnostic marker alongside clinical symptoms, ultrasound findings, and other hormonal tests.
4. Predicting Menopause
- Declining AMH levels are an early indicator of approaching menopause, often years before other hormonal changes occur.
- It aids in family planning and counseling regarding fertility preservation options such as egg freezing.
5. Monitoring Ovarian Surgery or Chemotherapy Effects
- AMH is useful in assessing post-surgical ovarian function and gonadotoxic effects of chemotherapy or radiotherapy.
- It helps determine the extent of ovarian damage and recovery potential.
Clinical Significance of AMH in Men
- In Infants and Children:
AMH helps evaluate testicular function in cases of ambiguous genitalia or cryptorchidism (undescended testes). - In Adults:
AMH testing is used in assessing Sertoli cell function and certain infertility conditions.
Diagnostic Importance and Laboratory Testing
1. Specimen Type
- Serum or plasma (EDTA or heparinized) samples are used.
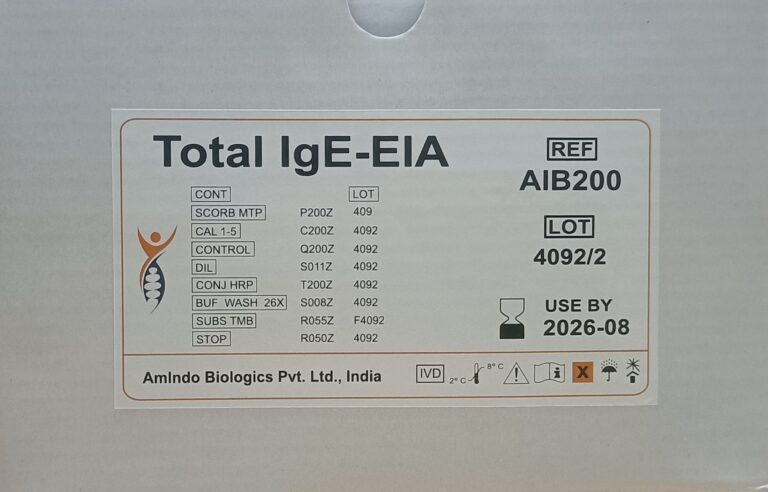
2. Method of Testing
- AMH is quantitatively measured using Enzyme-Linked Immunosorbent Assay (ELISA) or Chemiluminescent Immunoassay (CLIA) methods.
- High sensitivity and reproducibility make these techniques ideal for clinical use.
3. Reference Ranges
- AMH reference values vary with age, sex, and assay method, but generally:
- High AMH (>4.0 ng/mL): Suggestive of PCOS or high ovarian reserve.
- Normal AMH (1.0–4.0 ng/mL): Healthy ovarian function.
- Low AMH (<1.0 ng/mL): Reduced ovarian reserve or nearing menopause.
(Note: Reference ranges may differ based on laboratory and test kit manufacturer.)
Key Diagnostic Applications of AMH
| Clinical Application | Diagnostic Role |
| Assessment of ovarian reserve | Predicts fertility potential |
| PCOS evaluation | Elevated in PCOS cases |
| IVF planning | Determines ovarian stimulation response |
| Menopause prediction | Early indicator of ovarian aging |
| Monitoring after chemotherapy/surgery | Assesses ovarian recovery |
| Pediatric endocrinology | Evaluates testicular presence/function in male infants |
Advantages of AMH Testing
- Cycle-independent: AMH levels remain stable, so testing can be done any day of the menstrual cycle.
- Early indicator: Reflects ovarian status before clinical or ultrasound changes appear.
- Quantitative and reproducible: Reliable for serial monitoring.
- Predictive value: Strong correlation with fertility outcomes and ovarian health.
Conclusion
AMH testing has become an essential component in reproductive and fertility diagnostics. It not only reflects ovarian reserve but also provides actionable information for fertility management, PCOS evaluation, and menopause prediction. With advancements in immunoassay technologies like ELISA and CLIA, AMH testing offers high precision and clinical utility.
In both women and men, understanding AMH levels enables clinicians to make informed decisions, personalize treatment plans, and improve reproductive health outcomes.