Clinical Significance of Echinococcus Infection and Its Diagnosis
Introduction
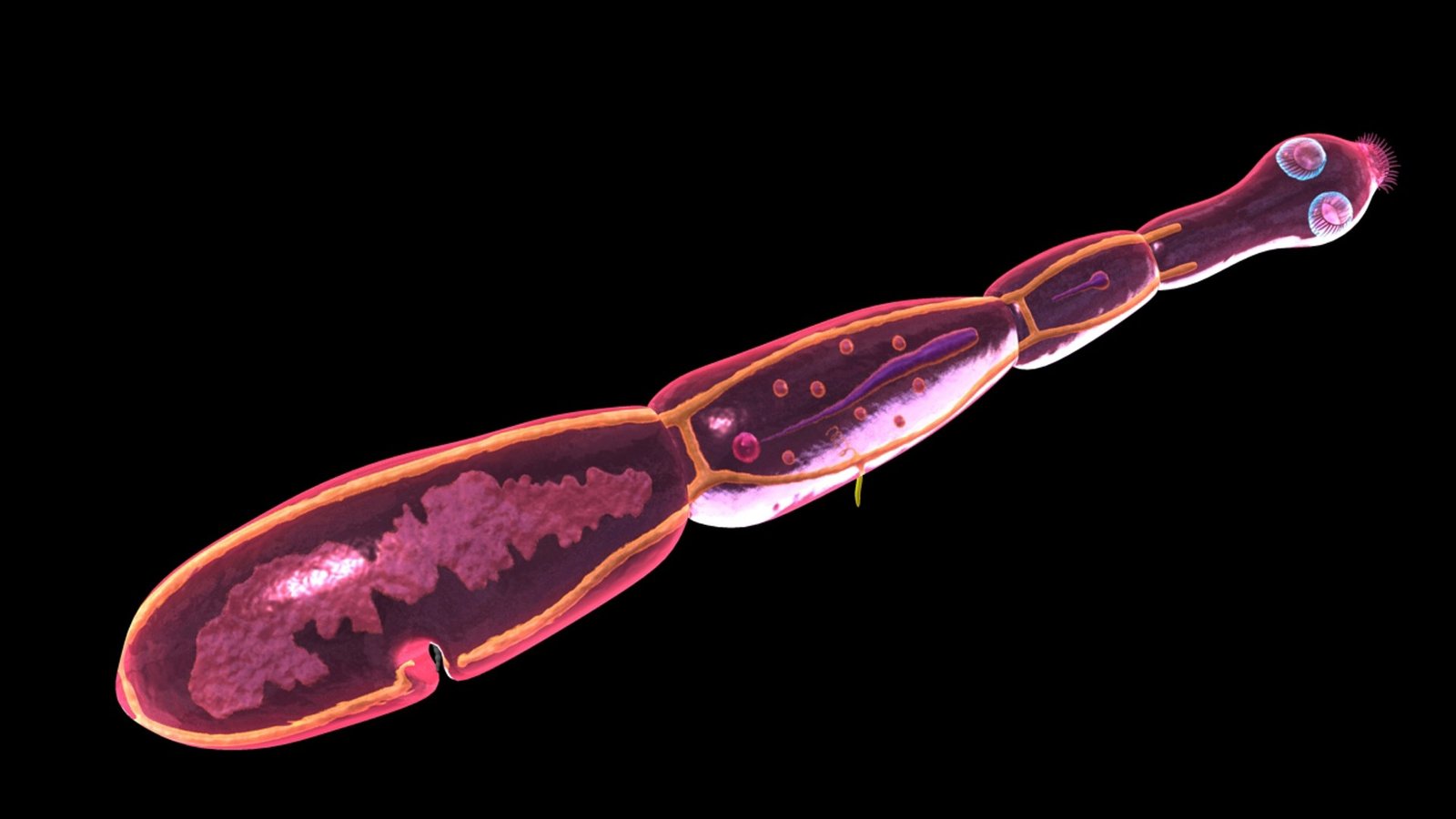
Echinococcus infection, commonly known as echinococcosis or hydatid disease, is a parasitic zoonosis caused by the larval stage of the tapeworm Echinococcus species. Despite being preventable, it remains a major public health concern in many developing and agricultural regions worldwide. The infection primarily affects the liver and lungs but can also involve other organs, leading to severe and sometimes life-threatening complications if left untreated.
Etiology and Transmission
The disease is caused by different species of Echinococcus, mainly:
- Echinococcus granulosus – responsible for cystic echinococcosis (CE)
- Echinococcus multilocularis – causes alveolar echinococcosis (AE)
- Less commonly, Echinococcus vogeli and Echinococcus oligarthrus cause polycystic forms.
Humans act as accidental intermediate hosts, acquiring infection through ingestion of Echinococcus eggs shed in the feces of infected dogs or wild canines. Once ingested, the eggs hatch in the intestine, and the larvae migrate through the bloodstream to various organs, developing into hydatid cysts.
Clinical Manifestations
The clinical presentation of echinococcosis varies depending on the site, size, and number of cysts.
- Liver involvement (70%): abdominal pain, hepatomegaly, nausea, or cyst rupture leading to anaphylaxis.
- Lung involvement (20–30%): chronic cough, chest pain, or hemoptysis.
- Other sites (10%): brain, bones, kidneys, spleen, and heart, presenting with organ-specific symptoms.
Due to its slow progression, the infection may remain asymptomatic for years, making early detection challenging.
Clinical Significance
Echinococcosis carries substantial morbidity and economic burden, particularly in endemic rural regions where close contact between humans and livestock facilitates transmission.
The significance lies in:
- Chronic disease burden: Progressive cyst growth can impair organ function.
- Surgical risks: Rupture of cysts during surgery can cause dissemination or anaphylactic shock.
- Public health impact: Affects livestock productivity and poses zoonotic risk.
- Need for accurate diagnosis: Early identification improves prognosis and helps prevent secondary infection.
Diagnostic Approaches
Accurate diagnosis requires a combination of imaging and serological techniques.
1. Imaging Methods
- Ultrasonography (USG): First-line tool for liver cysts; non-invasive and highly specific.
- CT/MRI scans: Provide detailed information on cyst location, size, and complications.
- Chest X-ray: Useful for pulmonary echinococcosis.
2. Serological Tests
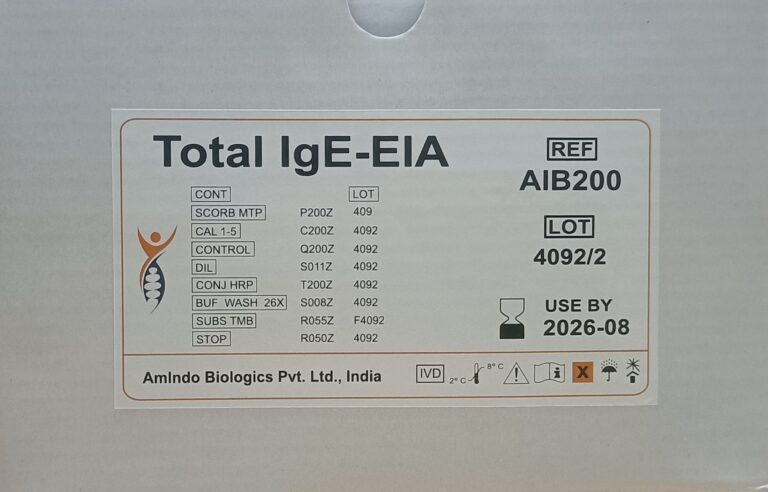
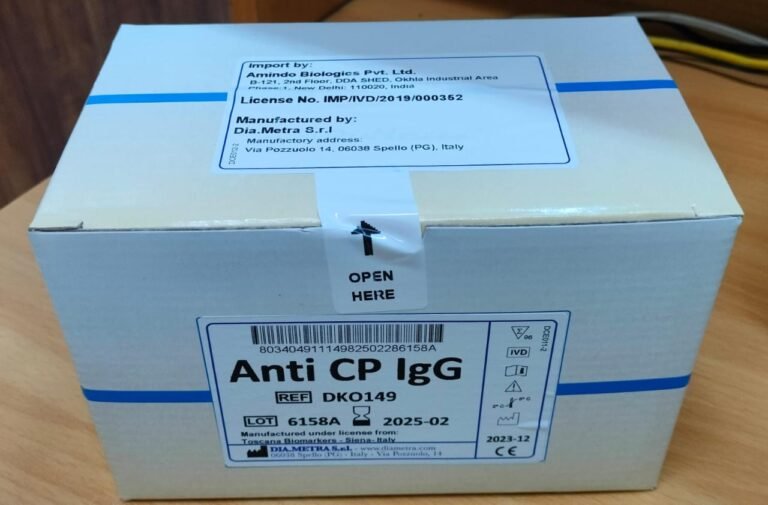
Serology plays a crucial role in confirming the diagnosis and monitoring treatment response.
Common assays include:
- ELISA (Enzyme-Linked Immunosorbent Assay): Detects Echinococcus-specific IgG antibodies; widely used for screening.
- Indirect Hemagglutination (IHA) and Immunoblotting: Provide higher specificity and help differentiate E. granulosus from E. multilocularis.
- Rapid Diagnostic Kits: Offer point-of-care solutions for field use and early detection.
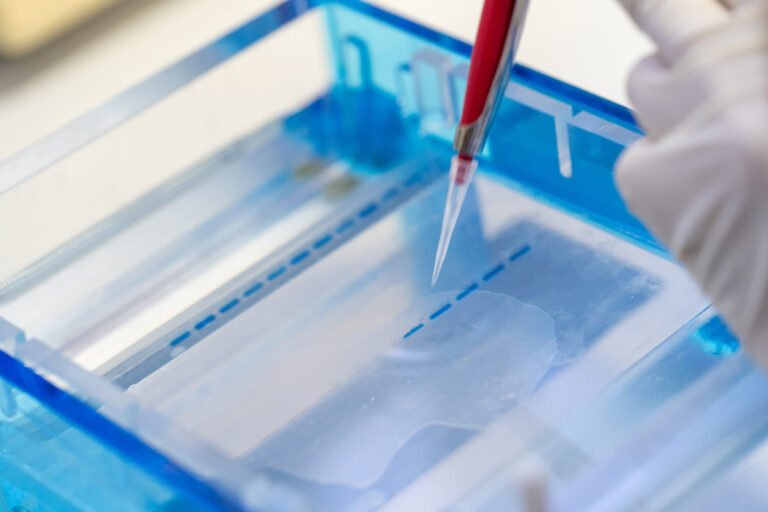
3. Molecular Methods
PCR-based assays enable direct detection of parasite DNA from tissue or cyst fluid, allowing species-level identification and epidemiological tracking.
Treatment and Management
Management depends on cyst type, size, and location. Options include:
- Medical therapy: Albendazole or mebendazole for small or inoperable cysts.
- Surgical intervention: For large or complicated cysts.
- PAIR technique (Puncture, Aspiration, Injection, Re-aspiration): Minimally invasive alternative to surgery.
Regular follow-up with imaging and serology helps assess treatment success and detect recurrences.
Conclusion
Echinococcosis remains a neglected tropical disease with serious clinical and socioeconomic implications. Early and accurate diagnosis is crucial for effective management and prevention of complications. Integration of serological, molecular, and imaging techniques can significantly improve detection and disease surveillance. Strengthening public awareness, veterinary control, and diagnostic accessibility is essential for reducing the global burden of this parasitic infection.