From Collection to Conclusion: HPV RT-PCR Test Workflow
Human Papillomavirus (HPV) infection is one of the most common sexually transmitted infections worldwide. Persistent infection with high-risk HPV strains can lead to cervical cancer, making timely detection critical. Among the various diagnostic techniques available, Real-Time Polymerase Chain Reaction (RT-PCR) is considered the gold standard for HPV DNA testing due to its high sensitivity, specificity, and reliability.
In this blog, we will walk you through the complete process of HPV testing — from sample collection to the final RT-PCR report.
1. Sample Collection
Accurate sample collection is the first and most crucial step for reliable HPV test results.
- Who collects the sample?
Trained healthcare professionals such as gynecologists, clinicians, or lab technicians. - Types of samples collected:
- Cervical swab or scrape – the most common method in women.
- Vaginal swab or urine sample – in some screening programs.
- Oropharyngeal or anal swabs – in specific high-risk populations.
- Collection process:
- A sterile cytobrush or swab is gently inserted into the cervix or target area.
- The brush collects epithelial cells, which may contain HPV DNA.
- The sample is placed into a transport medium, labeled properly, and stored at recommended conditions (usually 2–8°C) until testing.
Tip: Proper handling and avoiding contamination at this stage are critical for accurate results.
2. Sample Transportation and Storage
- Samples are transported in a Viral Transport Medium (VTM) or specialized collection medium.
- Cold chain maintenance is essential to preserve nucleic acid integrity.
- Samples must reach the laboratory within the stipulated time frame (generally within 72 hours).
3. Nucleic Acid Extraction
Once in the laboratory, the first technical step is the extraction of HPV DNA from the patient sample.
- Automated or manual extraction kits are used.
- The process removes inhibitors and isolates purified DNA for amplification.
- Quality control is performed to ensure sufficient nucleic acid yield.
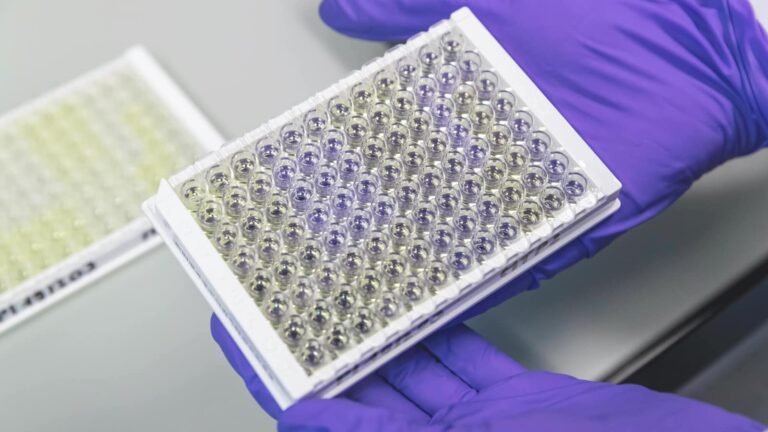
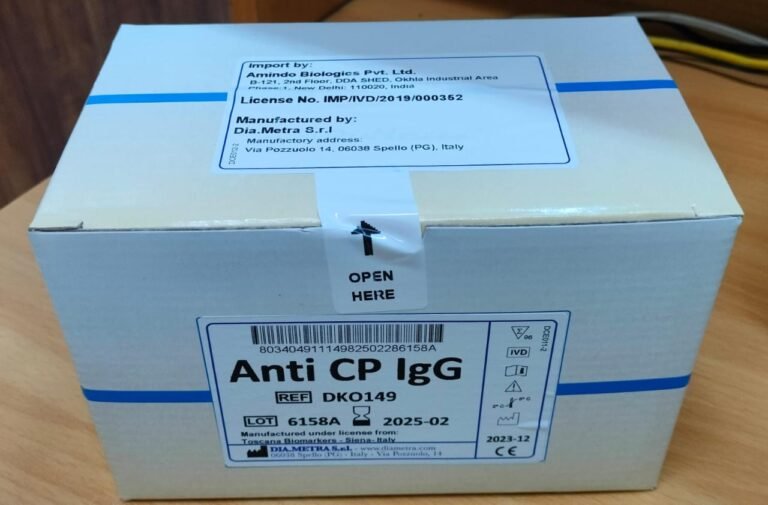
4. Real-Time PCR (RT-PCR) Amplification
RT-PCR is performed to detect and quantify HPV DNA.
- Principle:
The test amplifies HPV-specific DNA sequences using primers and probes. Fluorescent signals emitted during amplification are detected in real-time. - Steps involved:
- DNA template, primers, probes, nucleotides, and polymerase enzyme are added into a PCR reaction mixture.
- The PCR machine cycles through denaturation, annealing, and extension phases.
- Fluorescence signals increase proportionally with the amount of HPV DNA present.
- Targets:
- High-risk HPV genotypes (e.g., HPV 16, 18, 31, 45, etc.)
- Sometimes also detects low-risk HPV types depending on the kit.
5. Data Analysis and Interpretation
- The RT-PCR system generates Ct values (Cycle threshold) which indicate viral DNA presence.
- A low Ct value = higher viral load.
- Internal controls ensure no false negatives due to technical issues.
- Results are compared against assay-specific cutoff values.
6. Report Generation
The final report typically includes:
- Patient details and sample type
- Test methodology (HPV DNA by RT-PCR)
- Detected HPV genotype(s) or result as Positive/Negative for High-Risk HPV
- Clinical interpretation and recommendation for follow-up testing (e.g., Pap smear, colposcopy, biopsy).
7. Clinical Relevance
- Negative result: Indicates no high-risk HPV infection detected. Routine screening is advised as per guidelines.
- Positive result: Indicates the presence of high-risk HPV. Further evaluation by Pap smear or colposcopy may be required.
- Genotyping: Identifies specific HPV strains, which helps assess cancer risk more precisely.
Conclusion
From sample collection to the final RT-PCR report, HPV testing is a systematic process that requires precision and quality control at every stage. RT-PCR not only ensures early and accurate detection of high-risk HPV but also plays a crucial role in preventing cervical cancer through timely medical intervention.
Early screening, accurate diagnostics, and follow-up care are the cornerstones of reducing HPV-related cancer burden.