RIA-Based Technology in Healthcare Diagnostics
Introduction
In the ever-evolving world of medical diagnostics, precision and sensitivity are key to accurate disease detection. One of the pioneering techniques in laboratory medicine is Radioimmunoassay (RIA), a highly sensitive method used to measure minute concentrations of antigens, hormones, and other biological markers in blood and other body fluids. Even though newer technologies have emerged, RIA still holds a special place in the history and ongoing practice of clinical diagnostics due to its unmatched accuracy in certain applications.
What is Radioimmunoassay (RIA)?
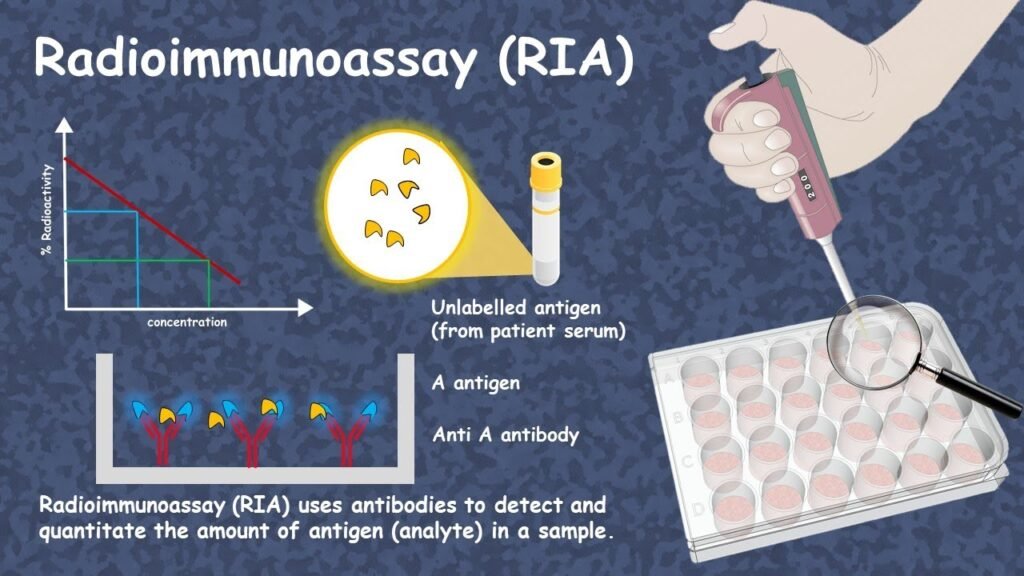
RIA is an in vitro assay technique that uses radioactive isotopes to detect and quantify specific substances in a sample. It is based on the principle of antigen-antibody binding and competitive inhibition. Developed in the 1960s by Rosalyn Yalow and Solomon Berson, RIA revolutionized diagnostic testing and even won Yalow the Nobel Prize in Physiology or Medicine in 1977.
How Does RIA Work?
The basic process of RIA involves:
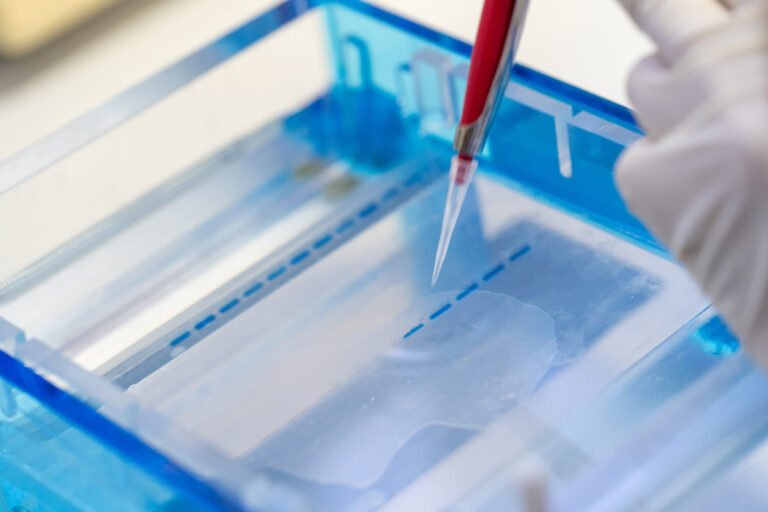
- Preparation of Antigen & Antibody – A known amount of radioactively labeled antigen is prepared.
- Competitive Binding – The patient’s sample containing an unknown amount of antigen competes with the labeled antigen for binding sites on a specific antibody.
- Separation – Bound and free antigens are separated using physical or chemical methods.
- Measurement – The radioactivity of the bound complex is measured using a gamma counter. The amount of radioactivity is inversely proportional to the concentration of the antigen in the patient’s sample.
Applications of RIA in Healthcare
RIA technology has been a gold standard in many diagnostic areas, including:
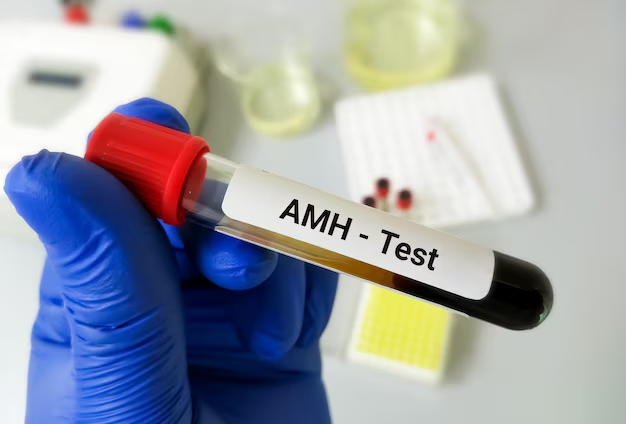
- Hormone Level Testing
- Thyroid hormones (T3, T4, TSH)
- Insulin and C-peptide
- Reproductive hormones (LH, FSH, estrogen, progesterone, testosterone)
- Infectious Disease Detection
- Hepatitis B surface antigen
- HIV markers (historically, before ELISA took over)
- Tumor Marker Detection
- Alpha-fetoprotein (AFP)
- Carcinoembryonic antigen (CEA)
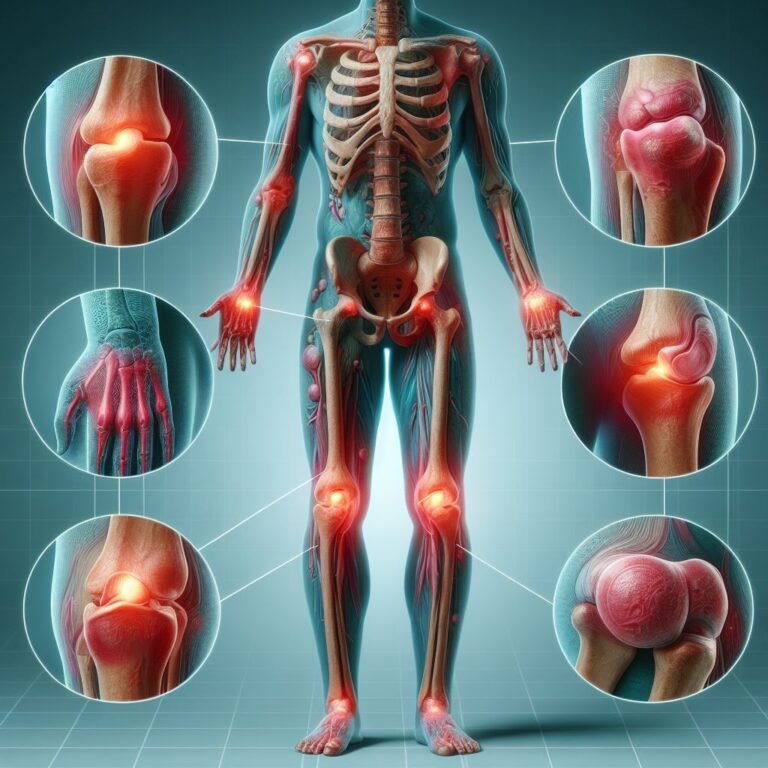
- Allergy & Autoimmune Testing
- Measurement of IgE levels
- Specific autoantibodies
Advantages of RIA
- High Sensitivity – Can detect substances at nanogram or even picogram levels.
- High Specificity – Uses highly specific antigen-antibody interactions.
- Proven Reliability – A long-standing method with decades of research backing its accuracy.
Limitations of RIA
- Radioactive Hazard – Involves handling and disposal of radioactive materials, requiring strict safety protocols.
- Regulatory Restrictions – Use of radioisotopes is heavily regulated.
- Labor-Intensive – Requires specialized equipment and trained personnel.
- Replacement by Modern Methods – In many cases, ELISA and CLIA (chemiluminescent immunoassay) are preferred due to safety and convenience.
RIA in the Modern Healthcare Landscape
While RIA usage has declined in favor of non-radioactive methods, it remains important in:
- Specialized research laboratories
- Hormone reference testing
- Certain niche diagnostic applications where ultra-high sensitivity is required
With proper safety measures, RIA continues to offer exceptional precision, making it invaluable in cases where other methods may fall short.
Conclusion
RIA-based technology laid the foundation for modern diagnostic testing by introducing unprecedented sensitivity and specificity. Though newer and safer techniques like ELISA and CLIA have largely replaced it in routine testing, RIA still plays a vital role in specific diagnostic and research applications. Its legacy in healthcare is undeniable — it not only transformed disease detection but also paved the way for advancements in personalized medicine and hormone research.