Diabetes Monitoring: Understanding Key Biomarkers for Effective Management
Diabetes is a chronic metabolic disorder that affects millions of people worldwide. Characterized by high blood glucose levels, the condition can lead to serious complications if not properly managed. Regular monitoring of blood glucose levels and key biomarkers is crucial in assessing the disease’s progression and determining appropriate treatment plans. In this article, we will explore four essential biomarkers used in diabetes monitoring: Insulin ELISA, C-Peptide ELISA, Anti-GAD, and IA2.
Insulin ELISA:
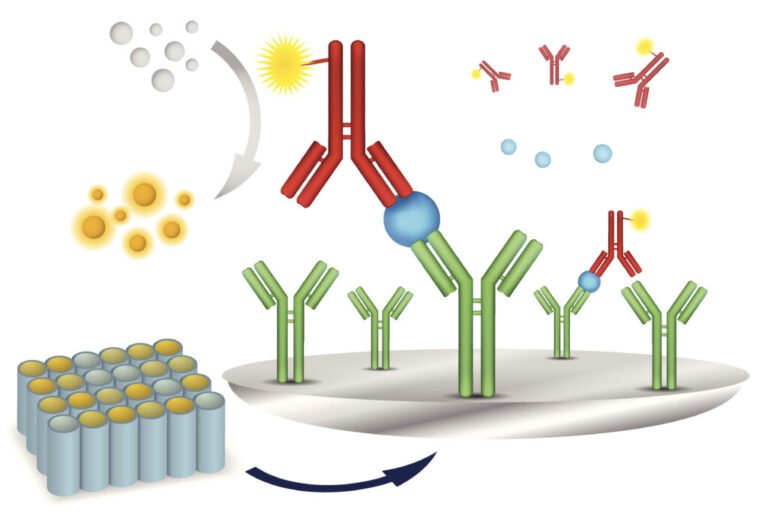
Insulin is a hormone produced by the pancreas that plays a central role in regulating blood sugar levels. In diabetes, the body either does not produce enough insulin (Type 1 diabetes) or is unable to use it effectively (Type 2 diabetes). The Insulin ELISA (Enzyme-Linked Immunosorbent Assay) is a laboratory test used to measure the concentration of insulin in the blood. It helps doctors determine if a patient is producing enough insulin or if exogenous insulin therapy is required.
For Type 1 diabetes patients, the Insulin ELISA helps monitor their insulin levels and adjust insulin dosages accordingly. For Type 2 diabetes patients, the test can assist in assessing their insulin resistance and guide treatment plans that may involve lifestyle changes, oral medications, or insulin therapy.
C-Peptide ELISA:
C-Peptide is a byproduct of insulin production. When the pancreas releases insulin, it also releases C-Peptide in equal amounts. Unlike insulin, C-Peptide is not metabolized by the liver, making it a reliable indicator of endogenous insulin secretion. The C-Peptide ELISA is a test that measures the concentration of C-Peptide in the blood.
This biomarker is particularly valuable in distinguishing between Type 1 and Type 2 diabetes. Type 1 diabetes is characterized by little to no insulin production, resulting in low C-Peptide levels. On the other hand, Type 2 diabetes patients often have normal or elevated C-Peptide levels, indicating that their pancreas is still producing insulin, but their bodies are resistant to its effects. This information guides physicians in determining the most appropriate treatment approach for each patient.
Anti-GAD (Anti-Glutamic Acid Decarboxylase):
Anti-GAD is an autoantibody directed against glutamic acid decarboxylase, an enzyme involved in the production of the neurotransmitter gamma-aminobutyric acid (GABA). Anti-GAD antibodies are commonly associated with Type 1 diabetes and certain neurological disorders. The Anti-GAD test measures the levels of these antibodies in the blood.
In Type 1 diabetes, the immune system mistakenly attacks and destroys beta cells in the pancreas, leading to insulin deficiency. The presence of Anti-GAD antibodies in the blood indicates an autoimmune response targeting the pancreatic beta cells. Early detection of these antibodies helps identify patients at risk of developing Type 1 diabetes, enabling early intervention and disease management.
IA2 (Insulinoma-Associated-2) Antibodies:
IA2 is another autoantibody linked to Type 1 diabetes. It targets an enzyme known as protein tyrosine phosphatase-like protein IA-2, which is also found in pancreatic beta cells. Similar to Anti-GAD, the presence of IA2 antibodies suggests an autoimmune attack on the beta cells and may indicate the onset or progression of Type 1 diabetes.
Monitoring IA2 antibodies, along with other autoantibodies like Anti-GAD, is essential in identifying individuals at high risk of developing Type 1 diabetes, especially in those with a family history of the condition. Early detection allows for timely intervention and potential enrollment in prevention studies to delay or prevent the onset of diabetes.
Conclusion: Diabetes monitoring plays a pivotal role in effective disease management. The use of key biomarkers like Insulin ELISA, C-Peptide ELISA, Anti-GAD, and IA2 helps healthcare professionals gain valuable insights into a patient’s insulin production, insulin resistance, and autoimmune response. Armed with this information, physicians can tailor treatment plans, make necessary adjustments, and provide personalized care to improve the quality of life for individuals living with diabetes. Regular monitoring of these biomarkers is vital in ensuring optimal diabetes management and minimizing the risk of complications associated with this chronic condition.